What is Sepsis?
- The word “sepsis” derives from the Greek which means to the Decomposition of animal or vegetable or organic matter in the presence of bacteria.
- The first use of sepsis in the medical context occurred over 2700 years ago in the poems of Homers.
- The term sepsis is derived directly from the word “sepo” which means “IROT”. At least 350,000 adults get sepsis and die either in the hospital or after release.
- One person dies from sepsis every 2.8 seconds around the world. It also known as septicemia or blood poisoning is a potentially life-threatening condition.
- Any type of infection can cause sepsis. e.g., Bacterial, Viral, Fungal. This disorder occurs when the body’s response to infection or injury while fighting causes the immune system to destroy its organs and tissues.
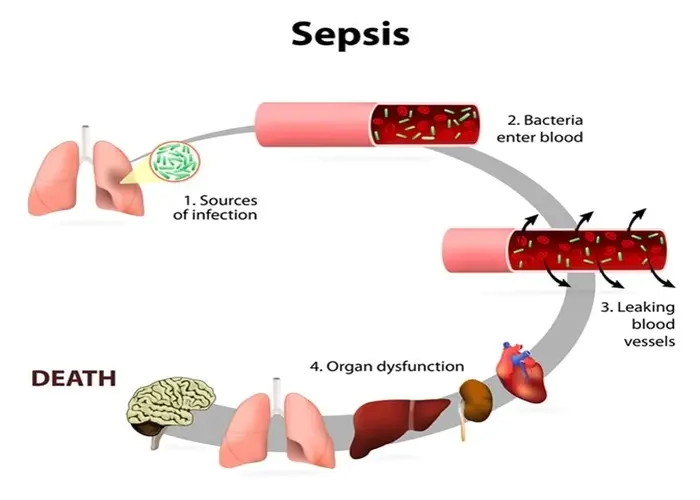
Image Source: News-Medical.Net
Who does sepsis affect?
Anyone can acquire sepsis from an infection. But some people are prone to have it. People with low immunity, such as
- Pregnant women.
- Elderly person older than 60.
- Infants less than 1 year old and who have any chronic disease, Including:
- Lever disease
- Heart, kidney
- Lung
- Uncontrol diabetes
- Leukaemia & Lymphoma & any type of cancer
- HIV
All of these chronic diseases increase the likelihood of developing sepsis.
Signs and symptoms of sepsis
The earliest signs of sepsis are often subtle and nonspecific and need a high index of suspicion for early diagnosis. Babies with sepsis may present the following symptoms.
Non-specific features of sepsis:
- Hypothermia or fever
- Lethargy
- poor cry
- Refusal to suck
- Poor perfusion
- prolonged capillary refill time
- Hypoglycemia
- Hyperglycemia
- Metabolic acidosis
Specific features related to various systems:
Gastrointestinal system:
- Feed intolerance
- Abdominal distention
- Vomiting
- Diarrhoea
- Hepatomegaly
Respiratory System:
- Apnea
- Dyspnea
- Tachypnea
- Rretractions
- Flaring
- Grunting
- Cyanosis
Renal System:
- Oliguria
Cardiovascular System:
- Pallor
- Mottling
- Cold
- Clammy skin
- Tachycardia
- Hypotension
- Bradycardia
Central Nervous System:
- Irritability
- lethargy
- Tremors
- Seizers
- Hyporeflexia
- Hypotonia
- Irregular respiration
- Full fontanel
- High-pitched cry
- Fever or low temperature
- Fast or slow heart rate
- Fast breathing or shortness of breath
- Diarrhea
- Reduced sucking/difficulty feeding
- Swollen belly (abdomen)
- Cold hands and feet
- Clammy, pale skin
- Yellow skin and whites of their eyes(jaundice)
- Reduced activity
Causes of sepsis
Bacterial infections are one of the most common causes of sepsis. Fungal, parasitic and viral infections are also potential sepsis causes. You can get sepsis when an infection triggers a chain reaction throughout your body causing organ dysfunction. The infection leading to sepsis can start in many different parts of the body. Common sites and types of infections that can lead to sepsis include:
1. Respiratory system: Infections involving your lungs, such as pneumonia.
Pneumonia:
- An infection of the lungs is called pneumonia.
- It may be caused by a fungus, viruses, or bacteria.
- As the lungs’ air sacs swell, one or both of the lungs may get damaged.
- Blood or fluid may fill the air sacs, resulting in fever, chills, coughing, and trouble breathing.
- Although pneumonia can strike anybody, the elderly, young children, and babies are the most vulnerable to its complications.
- There is a vaccine that lowers the likelihood of contracting the illness. On the other hand, the kind of organism that caused the illness will determine how pneumonia is treated.
a. Early-onset pneumonia: Develops within the first week of life and results from perinatal pathogen exposure, either intrauterine or during passage through the birth canal.
b. Late-onset pneumonia: It usually occurs after 7 days of age, most commonly in neonatal intensive care units among infants who require prolonged endotracheal intubation because of lung disease (called ventilator-associated pneumonia).
c. Congenital pneumonia: infection established during fetal life may result from an ascending infection across the chorioamniotic membranes or a hematogenous transplacental route.
2. Urinary tract system: Urinary tract infections are especially likely if you have a catheter.
3. Gastrointestinal system:
- Infection of your appendix (appendicitis).
- Bowel problems.
- Infection in your abdominal cavity (peritonitis).
- Gallbladder or liver infections.
4. Central nervous system: Infections of your brain or spinal cord.
5. Skin:
- Bacteria can enter your skin through wounds, inflammation or openings made with catheters and IVs.
- Conditions such as cellulitis (inflammation of your skin’s connective tissue).
Prevention of Sepsis
- Maternal infection is diagnosed and treated early.
- Isolation of infected babies.
- Prophylactic antibiotics for high-risk babies.
- Limitation of visitors and handling of the baby.
- Immunization.
- Parental education about the danger signs of newborns and the importance of hospital visits.
- Clean the environment of the neonatal unit and use sterile material before entering the unit and while handling the baby.
- Cots and incubators should be washed with soap and water and sterilized with cetrimide solution.
- Avoid unnecessary invasive procedures.
- Aseptic technique in an invasive procedure.
- Hygiene of the baby (sponging, cleaning, clothing).
- Handwashing before handling the babies.
- Infection control policies applied in the unit.
- Providing a clean place for birth.
- Delivering the baby within 12 to 24 hours of when membranes break (caesarean delivery should be done in women 4 to 6 hours or sooner of membranes breaking.)
- Use disposable tissues.
- Look, don’t touch.
- Avoid unwell people.
- Handwashing by birth attendants.
- Disinfection and sterilization of equipment.
- Minimization of vaginal examination and prompt diagnosis and treatment of prolonged labour.
- Preventing and treating infections in mothers, including HSV.
Neonatal Sepsis
- Neonatal sepsis is a critical condition that arises from a bacterial, viral, or fungal that occurs when a body under the age of 28 days develops a life-threatening response against infection
- The body generates inflammation, inflammation can spread through the body of a newborn and develop sepsis.
- It is associated with severe morbidity and mortality in the Neonatal period.
- It presents nonspecific clinical signs and symptoms such as respiratory distress, hypotension, and apnea.
- It is associated with pneumonia and other bacterial and viral infections.
- It is a serious condition in which pathogens infiltrate the bloodstream, multiply and produce toxins causing various effects on the health of neonates.
- It continues to be a common and significant healthcare burden, especially in very low birth weight infants (with birth weight less than 1500 gm.)
Who does neonatal sepsis affect?
- It can affect any baby, but premature babies develop sepsis more often than full-term babies because their immune systems are immature.
- Babies born prematurely do not have antibodies to protect them against bacteria. That’s because they’re born before they can receive the antibodies from their birthing parent.
Neonatal sepsis also more commonly occurs in babies:
- Those who have a low birth weight.
- Have a birthing parent with certain risk factors, such as an infection during pregnancy.
Neonatal sepsis is divided into three groups
- Early-onset neonatal sepsis
- Late-onset neonatal sepsis
- Very-late onset neonatal sepsis
1. Early-onset neonatal sepsis (EONS)
- EONS is a serious medical condition that occurs in newborn infants, usually within the first 72 hours of life. It is caused by a bacterial or fungal infection that the baby acquires during delivery, either from the mother’s genital tract or from the environment.
- Sepsis that develops before/within 72 hours after birth causes bacteria known as group B streptococcus.
Risk factors of EONS
Risk factors for EONS are divided into two groups based on risk.
1. Major criteria (closely related to neonatal sepsis)
- Chorioamnionitis is one of the most important risk factors in EONS.
- It is defined as an acute inflammation of foetal membranes and amniotic fluid.
- It often Develops due to the micro invasion of amniotic fluid as a result of prolonged rupture of membranes for more than 18 hours.
- Maternal temperature before or during labour>38 C, premature rupture of membranes before 37 weeks, and maternal group B streptococcus infections colonisation.
- Low birth weight
- Low levels of transplacental maternal IgG level in preterm babies
- Foetal distress
- Multiple pregnancies
- Resuscitation of the baby
2. Minor criteria (not related to neonatal sepsis)
- Including membrane rupture lasting over 12 hours but less than 18 hours.
- Spontaneous prematurity lasting less than 37 weeks but more than 35 weeks, Irregular foetal heartbeat or unexplained foetal hypoxia.
- The presence of one of these criteria requires clinical observation, especially during the first 24 hours after birth.
- Birth weight and gestational age are negatively associated with infection and death.
- Microorganisms in the maternal urogenital and digestive tracts have been linked to the EONS.
- Streptococcus agalactiae (Group B streptococcus) and Escherichia coli are the second culprits.
2. Late-onset neonatal sepsis (LONS)
- Sepsis, which develops after 72 hours of life, is slowly progressive.
- It occurs in very low birth weight infants.
- It usually occurs via the transmission of pathogens from the surrounding environment after delivery, such as contact with healthcare workers or caregivers.
- Neonatal Sepsis occurs in less than 1 year of children
Risk factors of LONS
Hospital-acquired infection in the hospital environment, several factors enhance the risk of neonatal sepsis. These include:
- Prematurity low birth weight
- Invasive medical procedure
- Mechanical ventilation
- Poorly disinfected hands and equipment
Community-acquired infection. These include:
- Bottle feeding
- Poor umbilical cord care practices
- Poor hygiene of the hands
- The importance of lactation in reducing postnatal infection was demonstrated.
- Frequent blood sampling
- Incubation
- Mechanical ventilation
- Catheter/probe insertion
- Insufficient breastfeeding
- Long-term parenteral nutrition
- Low stomach acid and
- Surgical interventions especially increase the risk of LOSN
3. Very-late onset neonatal sepsis (VLONS)
- VLONS is a bacterial infection that occurs in newborns after the first week of life, usually between 7 and 90 days after birth.
- It is a serious medical condition characterised by bacteria or other infectious agents in the bloodstream of a newborn baby, causing systemic infection.
- It is often caused by Candida species or by commensal organisms.
- Risk factors for VLONS may include prolonged hospitalisation, exposure to invasive medical procedures, and other factors that compromise the infant’s immune system. Premature infants and people with underlying health problems may be especially vulnerable.
Complications of Neonatal Sepsis
Some possible complications of neonatal sepsis are:
- Kidney failure.
- Tissue death of fingers or toes that may require amputation.
- Permanent lung damage from acute respiratory distress syndrome.
- Permanent brain damage, which can cause memory problems or more severe symptoms causes meningitis.
- Later problems with the immune system can raise the risk of future infections.
- Newborns with bacterial meningitis are usually irritable, vomit, extreme sluggishness, seizures and coma.
- Damage to the heart valves (endocarditis), which can lead to heart failure.
Diagnosis of Neonatal Sepsis
An infection can start with a simple injury like a shallow cut on the arm that allows bacteria & other microbes to enter into the body’s tissues or circulation. The immune system is designed to defect these foreign invaders, launch an attack, and kill the infectious microbes, but sometimes the defence doesn’t work as planned. A single diagnostic test for sepsis does not yet exist, doctors & healthcare professionals use a combination of tests immediately.
Tests are included to diagnose the sepsis
- Blood test
- Compete blood count
- CRP (C-reactive protein)
- Lactate
- Urine test chest X-ray
- Ultrasound
- Blood culture
1. Blood tests:
For patients with possible signs of sepsis, several blood tests can be utilized. Even though these tests cannot diagnose sepsis, combining the results with other information can help.
Some of the different blood tests that can be employed include:
CBC:
A low WBC count (< 5,000/µL) is associated with a higher likelihood ratio for sepsis than an elevated WBC count (>20,000/µL). A differential may be of use in diagnosing sepsis; however, these counts are largely dependent on the laboratory and the technician performing them. One of the key techniques of a CBC test in the context of sepsis diagnosis is obtaining the WBC count, as these cells help fight microbes in the blood.
Lactate: Lactate levels reflect the presence of lactic acid in the blood, which is an indication of low oxygen.
CRP (C- reactive protein): It indicates the inflammation of the body. The most commonly used cut-off value for CRP during the first days of life continues to be 10 mg/L by use of ROC (receiver operating characteristic) analysis we demonstrated that CRP could play a role in the early diagnosis of neonatal sepsis if cut-off values were lowered.
PT and APTT, Platelet and D-dimer tests: Each of these tests is used to assess blood clotting activity in the blood. PT and APTT indicate poor blood clotting.
Low platelet levels indicate unseen clotting in tiny vessels all over the body. An indication of one large clot or many small clots in the body is identified by the high level of D-dimer.
Confirmatory examinations: Three types of blood testing can confirm sepsis:
a. Endotoxin test: The presence of endotoxin in the blood verifies the presence of gram-negative bacteria; however, this test cannot identify the exact type of bacteria.
b. Procalcitonin (PCT) test: A low PCT level in the blood indicates that the condition is not caused by bacteria, but rather by a viral infection or a non-infectious illness.
c. SeptiCyte test: This test determines whether or not the products of sepsis related enzymes are active.
2. Urine examination: In situations of sepsis, two types of urine tests are ordered:
a. Urinalysis: This procedure detects the existence of a urinary tract infection, and additional abnormalities that might arise within the kidneys.
b. Urine culture: A urine culture can be used to identify the bacteria or fungi that are causing the UTI.
3. Examinations for related medical conditions: In addition to blood and urine testing, additional tests relating to various conditions that can cause sepsis to occur. Some examples include, but are not limited to:
Micro-ESR: It is simple, but not very reliable. A value >15mm in 1st hour is suggestive of infection.
Gastric aspirate: Microscopic examination and culture of material obtained from gastric aspiration for leukocytes and bacteria are useful in identifying infants who are at risk of sepsis.
Blood culture: It is the gold standard for the diagnosis of septicaemia and should be done in all cases of suspected sepsis before starting antibiotics. A positive blood culture and sensitivity of the isolate is the best guide to antimicrobial therapy.
4. Imaging tests:
- For pneumonia, a chest X-ray, pulse oximetry, and a sputum test are performed.
- For meningitis, a lumbar puncture, magnetic resonance imaging (MRI), and computerized tomography (CT) scan are performed. • A rapid antigen test and a throat examination are also performed.
- Rapid influenza diagnostic testing and culture for strep throat for influenza symptom analysis.
- Skin culturing for skin infections
Therefore, sepsis diagnosis in neonates is typically based on a combination of maternal risk factors, haematologic indices and the judgement of the physician rather than their clinical presentation.
Early biomarkers combined with an accurate one of the widespread laboratory markers of infection (C reactive protein (CRP), white blood cell count (WBC), absolute neutrophil count (ANC), immature to total neutrophil ratio (IT-ratio) has enough sensitivity or specificity to detect all infected children. Their diagnostic value might be especially limited in the early course of the disease.
The limitations of microbial cultures are resolved by the development of high-sensitivity molecular diagnostic methods. The early identification of the pathogen-specific nucleic acid is the aim of these innovative methods.
Pediatric Sepsis
- Pediatric sepsis is a serious and potentially life-threatening condition in children that results from the body’s overreaction to infection.
- Sepsis occurs when the body’s immune system, instead of effectively fighting an infection, triggers a widespread inflammatory response that can lead to organ dysfunction and failure.
- It is a medical emergency that requires prompt recognition and intervention.
- It is a complex and dynamic condition, and the approach to diagnosis and management may vary depending on the child’s age, underlying health conditions, and the specific infectious agent involved
- Timely intervention and close monitoring are essential to improve the outcomes of children with sepsis.
- It occurs at less than 14 years in children.
- It remains an important cause of morbidity and mortality in children.
- It is a clinical syndrome caused by a dysregulated host response to severe infection.
Bacterial infections are the most common cause of pediatric sepsis. Common bacteria are:
- Staphylococcus aureus
- Escherichia coli
- Listeria monocytogenes
Effects on childhood:
- Severe pneumonia
- Severe diarrhoea
- Severe malaria
References
- https://link.springer.com/book/10.1007/978-3-319-48470-9
- https://www.ncbi.nlm.nih.gov/books/NBK430939/
- https://www.mdpi.com/books/book/4709-new-strategies-for-treatment-of-sepsis

